Connect With Us
Blog

Causes and Symptoms of Foot Blisters

Blisters, those tiny pockets of annoyance that can develop on the feet, are often the result of friction, heat, and moisture conspiring against our skin. Blisters form as a protective response, shielding the delicate layers of skin beneath from further damage. Ill-fitting footwear, especially new shoes that have not been properly broken in, are common culprits. Extended periods of walking, running, or any repetitive motion can exacerbate the friction, triggering blisters. Additionally, sweaty feet trapped in damp environments provide the ideal environment. The symptoms are tender, swollen patches of skin filled with clear fluid, which may eventually rupture, leaving raw skin exposed. While prevention through comfortable footwear and moisture-wicking socks is key, understanding the causes and symptoms equips you to treat blisters promptly and prevent their unwelcome intrusion. If you frequently develop blisters on your feet, it is suggested that you contact a podiatrist who can provide you with additional prevention techniques.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact Tanya R. Sellers-Hannibal, DPM of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are pockets of fluid that occur under the top layer of your skin. These fluid pockets are usually filled with pus, blood, or serum. Blisters may itch or hurt and can appear as a single bubble or in clusters.
The most common types of blisters are friction blisters. This type of blister may be caused by wearing shoes that are too tight. Friction blisters can also occur on the hands. A change in temperature may also cause blisters on the feet. In the freezing air, frostbite on your toes can lead to blisters, as well as sunburn from hot weather.
The best way to treat a blister is to keep it clean and dry. Most blisters will get better on their own. Once the skin absorbs the fluid within the blister, it will flatten and eventually peel off. You should avoid popping your blister unless you podiatrist does it for you. Additional treatment options include applying an ice pack to the blister or using over-the-counter blister bandages to cover the affected area.
If your blister becomes discolored, inflamed, or worsens it is advised that you speak to your podiatrist. Blisters that are yellow, green, or purple may be infected and require immediate medical attention. Blisters that are abnormally colored may be a sign of a more serious underlying health condition such as herpes.
Causes of Cracked Heels

Cracked heels are a common foot ailment stemming from dry and thickened skin around the heel edge. While they often cause cosmetic concerns, they can also trigger discomfort and pain. When left untreated, cracked heels may even lead to infection. Studies indicate that among adults who have encountered cracked skin on their feet, women report the condition more frequently than men. Deep cracks can be painful and bleed, particularly while standing. Obesity, wearing ill-fitting shoes, and prolonged standing can contribute to developing cracked heels. The skin's lack of moisture and decreased elasticity, especially under the heel's fat pad, can worsen the situation. Additional culprits include wearing open-back or poorly fitting shoes, friction, improper gait, and dry, cold weather. Additionally, athlete's foot, fungal infections, and heel spurs can significantly contribute to getting cracked heels. Countermeasures involve moisturizers, keratolytic creams, cotton socks, and liquid bandages. If soreness, redness, swelling, or severe pain from cracked heels persists for days, it is suggested that you consult with a podiatrist for a consultation and treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Tanya R. Sellers-Hannibal, DPM from Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Lyme Disease and the Feet

Lyme disease, often transmitted by ticks, can bring about various symptoms that affect the feet and other parts of the body. While fever, fatigue, and rashes may signal its presence, a definitive diagnosis requires careful consideration of symptoms and circumstances. If one has been in wooded or grassy areas during tick season, it is possible to contract Lyme disease. Lyme disease's early signs, such as fever, chills, headache, fatigue, and muscle pain, can mimic a severe cold. Knee swelling is common, and joint pain may migrate across the body. As the disease progresses, headaches, Bell's palsy, and joint pain can intensify, and rare complications like heart involvement or mental health issues may arise. Shooting pains, numbness, or tingling in the hands and feet may be felt. It is suggested that you manage pain and inflammation and focus on your overall well-being to aid in healing. If you suspect you have Lyme disease, it is suggested that you make an appointment with a podiatrist for an accurate diagnosis and effective management.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact Tanya R. Sellers-Hannibal, DPM from Maryland. Our doctor will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
Foot Surgery for Rheumatoid Arthritis May Improve Mobility

Rheumatoid arthritis, abbreviated RA, is a chronic autoimmune condition that can severely impact the joints, including those in the feet. When conservative treatments fail to provide adequate relief, foot surgery becomes a viable option for managing RA and related foot deformities. Surgical procedures aim to correct joint alignment, reduce inflammation, and improve overall foot function. Common surgical interventions for RA in the feet include a synovectomy, which is the removal of the inflamed joint lining, tendon repair or transfer, joint fusion, and joint replacement. It's important to note that foot surgery for RA is considered a last resort when other treatments have proven ineffective. It is beneficial for patients to work closely with their podiatrist to determine the most suitable surgical approach based on individual needs and medical history. While foot surgery may involve a recovery period, it can significantly enhance mobility, reduce pain, and ultimately improve the quality of life for those living with RA. It is suggested that you consult with a podiatrist if this condition affects you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Tanya R. Sellers-Hannibal, DPM of Maryland. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot and Ankle Surgery
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.
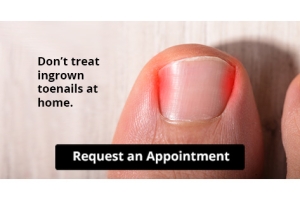
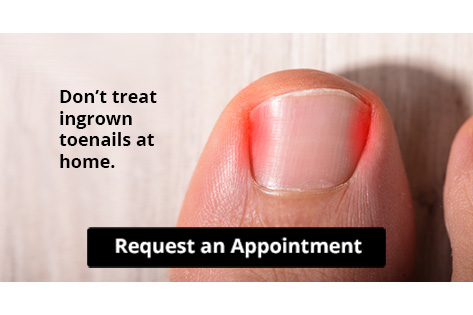
Let the Expert Treat Your Ingrown Toenails
Reasons Why the Feet Can Swell

Swollen feet are a common foot condition. There are several causes of swollen feet, and relief may be found when determining the source of the problem. Lifestyle factors may contribute to getting swollen feet, which can range from eating habits to pregnancy. Some patients are afflicted with chronic venous insufficiency, which is a condition that limits blood flow from the feet to the heart. Having swollen feet may also characterize an infection and can be common among diabetic patients. Serious ailments involving blood clots can be known to cause swollen feet and ankles, and immediate medical attention is often sought. Additionally, swollen feet may indicate heart disease, which may cause the blood to back up and pool in the feet and ankles. If you have swollen feet, it is strongly suggested that you are under the care of a podiatrist who can effectively treat this condition.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact Tanya R. Sellers-Hannibal, DPM of Maryland. Our doctor can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please feel free to contact our office located in Owings Mills, MD . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.